
By Arnold Ageta
One night, two years ago in the leafy village of Mwongori, screams filled the air on a chilly evening, bringing with them bad tidings: a newborn baby and mother had died.
The baby passed away the same day it was born, never having tasted the oxygen the earth could offer, while the mother struggled in labor.
James, not her real name, suffered a double loss that shattered his wild expectations of holding a baby boy in his hands.
His wife had visited a local hospital, expecting to give birth like any other expectant mother. Accompanied by her husband (James), she was booked and admitted.
James then left for home as his sister-in-law arrived to care for his wife. Departing the hospital excitedly, James held high hopes for finally welcoming a baby boy, confirmed through the three scans conducted prior to delivery.
Little did he know it would be the last time he saw his wife alive. That very night, both the baby and his wife succumbed to labor pains.
His sister-in-law claims the nurses were arrogant and careless, prolonging her sister’s agony, which ultimately led to the tragic outcome.
“The nurses were reluctant to attend to her, insisting she dilates to a certain centimeter before receiving help,” said James.
In the agonizing wait, she collapsed and was rushed to surgery. “She didn’t survive. She passed away,” he said with tears in his eyes. “They tried to save the baby, but it was too late.”
James says the ignorance of the nurses led to the death of his wife and the baby, leaving a permanent scar in his heart.
If the nurses responded to her wife’s cries, he says, she would be alive today. He adds that what his wife went through is a painful death that she did not deserve.
“I thought hospitals are safe delivery facilities but what women undergo in those maternity wards are traumatizing and torturing,” he said wiping his eyes.
He wonders “why would women suffer in the hands of their fellow women during the delivery process” yet they are the one who have been entrusted with safe delivery.
Such experiences have smeared evil and dirt not only on public hospitals but also faith-based hospitals in the country.
Many women have reported ignorance, arrogance, abusive, mishandling and mistreatment in maternity wards something that has often gone undealt with by relevant authorities.

In a recent study by Nguvu Collective, titled “Towards Ending OBV in Kenya” – Unveiling the Invisible Wounds of Obstetric Violence Through the Voices of Kenyan Women,” attempted to unveil the prevalence of Obstetric Violence (OBV) in Kenya.
In its survey, they drew responses from 189 women from 27 counties in 7 provinces of the country.
Findings indicate that 83 percent of the respondents had experienced at least one form of OBV where 11 per cent were women living with disabilities.
The study further discovered that 46 per cent of women who had experienced OBV were between 25 and 34 years of age.
It was found out that many women experience psychological and emotional abuse such as disregard of needs and pain, verbal abuse and humiliation, dehumanizing and rude treatment, and discrimination. This form of OBV is most common in public health facilities where many cases go unreported due to fear and accounts for 62 per cent.
The second form that featured in the study is medical neglect, malpractice, and unnecessary interventions such as denial of care, unsanitary maternity settings, non-consensual pelvic exams and forced sterilizations.
Another issue raised on this form of OBV included, unnecessary cesarean sections performed without medical justification, and unnecessary/wrong medication prescription and recommended usage. This form of OBV, according to the study accounted for 28 per cent.
“Physical violence and coercion such as pressuring or manipulating women into accepting medical interventions or procedures they do not want or need, hitting, slapping, kicking, or restraining a woman during pregnancy, childbirth, or the postpartum period account for 10 per cent,” the report revealed.

The study pointed out when and at what stage of pregnancy OBV happened where more than half of the respondents said the experienced it during child birth.
The women, 55 per cent claimed to have been mistreated at this stage. Additionally, 27 per cent of incidents occurred during pregnancy, highlighting that mistreatment is not confined to the labor and delivery process.
“A notable proportion of incidents, 14 per cent, occurred during the postpartum period, underscoring the importance of addressing obstetric violence throughout the entire continuum of care,” read the report.
In terms of the period when they experienced OBV, 33 per cent of the respondents reported that they had experienced OBV between 2018 – 2021, while the rest reported to have experienced OBV in the periods between 2022 – 2024 (30%), 2014 – 2017 (14%), 2010 – 2013 (13%), and the period before 2010 (14%).
“The period 2018-2021 aligns closely with the onset and progression of the COVID-19 pandemic globally which caused disruptions in healthcare services, resource constraints, and increased stress on healthcare workers,” the report suggested.
These factors could have contributed to an environment conducive to obstetric violence which might explain the increased incidents.
“While 59 per cent of women respondents experienced OBV at public hospitals, 16 per cent sought care at private hospitals. Additionally, OBV incidents occurred in a variety of healthcare settings, including health centers at a rate of 4 per cent, maternity clinics at 2 per cent, and mission/faith-based hospitals at 5 per cent,” the study revealed.
“This data suggests that OBV is not limited to any specific type of healthcare institution, indicating the need for further research with a larger and more diverse sample size to understand better which institutions may be more prone to OBV,” stated the report.
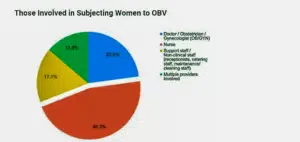
Multiple healthcare providers were reported to be involved in OBV. However, those most involved in subjecting women to OBV were found to be nurses who accounted for 51 per cent, doctors/obstetricians/gynecologists (25%), and support/non-clinical staff (19%) such as receptionists, catering staff, maintenance and cleaning staff.
The study illustrated that 68 per cent of the OBV incidents violated the patients’ human rights which included physical abuse, verbal abuse, forced procedures, withholding information, ignoring or dismissing concerns, denial of care, lack of privacy and dignity, discrimination, and failure to follow protocols or guidelines.
It is unfortunate that 9 per cent of the incidents reportedly resulted in infant death, while 13 per cent had a long-term negative impact on the child’s health and development.
“13 per cent of the women reported that they were harmed and had physical injuries during childbirth as a result of OBV,” read the study.
This study has also revealed that almost all incidents are not reported due to individual decision feeling that nothing will be done about it.
“Fear of retaliation or further mistreatment was also a significant deterrent, impacting 32 per cent of survivors,” the study stated. “Many attributed lack of awareness of how and where to report and lack of confidence in the reporting process were other key factors contributing to underreporting,” said the report.
Additionally, the report states that: “Feelings of stigma or shame, concerns about confidentiality or privacy, and the perception that obstetric violence was a normal experience for women also influenced survivors’ decisions not to report incidents.”
United Nations Population Fund (UNFPA) Kenya puts Kenya’s says that the number of women dying of pregnancy-related causes, stands at 355 deaths per 100,000 live births.
While access to skilled birth attendance has improved from 62 per cent to about 70 per cent over the last seven years, over 80 per cent of maternal deaths are attributed to poor quality of care.
Additionally, many more women and girls survive with severe morbidity including obstetric fistula and mental health complications.
Meanwhile, WHO statistics indicate that globally, a woman dies of pregnancy-related causes every two minutes and most of these are deaths are preventable with the right care at the right time.



